AI predicting pediatric cancer recurrence represents a groundbreaking advancement in the field of medicine, particularly in the treatment of brain tumors. Recent studies have shown that artificial intelligence tools can surpass traditional methods by analyzing brain scans over time, significantly improving the predictive accuracy for relapse in pediatric cancer patients. For conditions like glioma, where recurrence risk varies widely, this development could revolutionize pediatric cancer management. The integration of machine learning healthcare techniques allows for early identification of at-risk patients, potentially leading to less burdensome follow-up procedures for families. As we harness AI in medicine, we move closer to tailored treatment plans that could optimize brain tumor treatment outcomes for children.
The potential of artificial intelligence in forecasting the re-emergence of pediatric cancers offers new hope for improving healthcare outcomes. Current research highlights the efficacy of machine-learning algorithms that analyze sequential imaging data, enabling healthcare professionals to assess glioma recurrence risks accurately. As pediatric oncology evolves, the insights gleaned from continuous patient monitoring may enhance the understanding of individual tumor behavior. By transitioning from conventional diagnostic methods to innovative techniques utilizing AI, we can mitigate the psychological and physical burden on young patients and their families. The future of brain tumor treatment is poised to embrace more sophisticated approaches, ensuring that pediatric patients receive the most personalized and effective care possible.
Understanding Pediatric Cancer Recurrence Risks
Pediatric cancer, particularly brain tumors such as gliomas, poses unique challenges due to the risk of recurrence even after seemingly successful treatment. As treatments advance, understanding the specific recurrence risks associated with these tumors becomes increasingly vital. With survival rates improving, the focus has shifted to not just curing, but also effectively managing long-term outcomes. This is where artificial intelligence (AI) plays a crucial role, leveraging machine learning healthcare techniques to analyze vast amounts of data that can paint a clearer picture of individual patient risks.
Research has consistently shown that many pediatric gliomas can be treated effectively with surgery. However, the unpredictability of relapse remains. Factors influencing recurrence include tumor grade and the age of the patient at diagnosis. By integrating AI tools trained on comprehensive datasets, healthcare professionals can better stratify patients based on their risks of relapse, enabling more tailored monitoring and treatment strategies. This proactive approach is essential for improving the quality of life for young patients and their families.
AI’s Role in Predicting Pediatric Cancer Recurrence
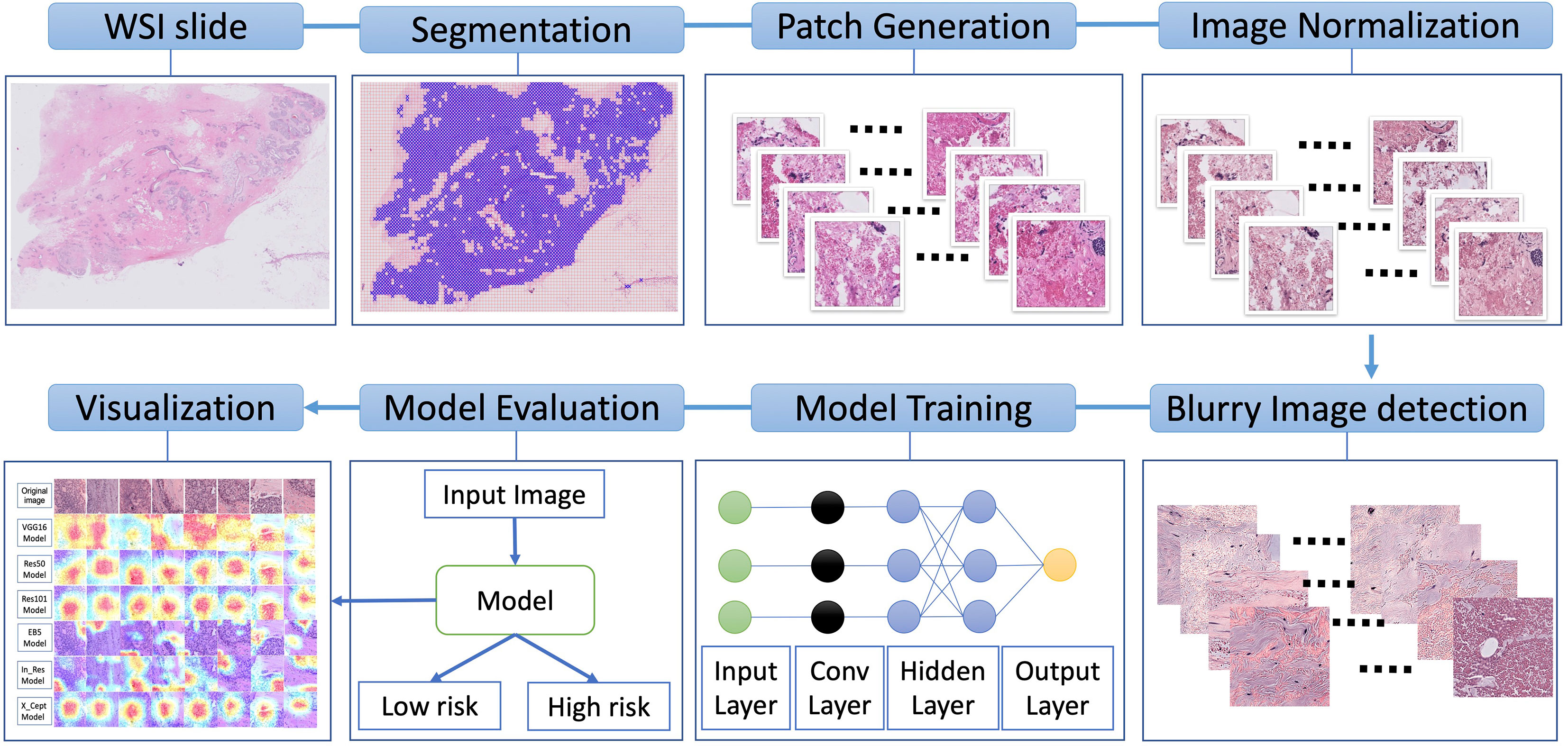
Recent studies highlight the revolutionary potential of AI in predicting pediatric cancer recurrence, especially in cases of glioma. Traditional methods often rely on limited and static data, which can lead to missed opportunities for early intervention. However, AI tools utilizing temporal learning can analyze multiple brain scans over time, reliably identifying changes that occur long before clinical symptoms arise. This capability not only enhances prediction accuracy but also allows for more personalized care pathways for young patients.
The integration of AI predicting pediatric cancer recurrence marks a significant advancement in patient management. As systems become more sophisticated, healthcare providers can expect higher predictive accuracy rates, thus optimizing follow-up protocols. For instance, AI-driven insights could indicate a lower frequency of imaging for patients identified as being at lower risk, ultimately alleviating the emotional and financial burden of frequent hospital visits for families. This transformation in how pediatric cancer is monitored and treated showcases the profound impact of AI on improving healthcare outcomes.
Temporal Learning and Its Impact on Glioma Management
Temporal learning represents a groundbreaking approach within the realm of AI in medicine, specifically for managing glioma recurrence risks in pediatric patients. By arranging and analyzing a sequence of brain scans over time, this technique has proven to significantly enhance the predictive capabilities of AI models. The ability to track subtle changes across multiple scans enables a deeper understanding of tumor behavior—information that static, single-scan analysis simply cannot provide.
Through temporal learning, researchers have shown that predicting glioma recurrence one year post-treatment can reach accuracies between 75-89 percent. This is a considerable improvement compared to traditional methods, which hover around 50 percent accuracy. Such advancements not only support clinical decision-making but also empower healthcare providers to develop more proactive treatment correlations. As the field progresses, additional validations and clinical trials will be crucial to confirm these findings and fully integrate temporal learning into standard care.
Challenges of Traditional Monitoring Techniques
Traditional methods of monitoring pediatric cancer recurrence involve frequent scans and consultations, often leading to anxiety and stress for patients and families. The reliance on standard imaging techniques sometimes fails to account for the nuanced changes that precursors to relapse may indicate. As a result, young patients may endure unnecessary procedures, impacting their emotional well-being and quality of life. Furthermore, health systems face logistical burdens due to scheduling, costs, and resource allocation.
The shortcomings of conventional monitoring underscore the need for more sophisticated approaches like AI. By employing advanced machine learning algorithms, healthcare providers can streamline monitoring processes, reducing the number of unnecessary scans while still ensuring that high-risk patients receive the vigilant oversight they need. This shift not only promotes a better patient experience but also facilitates a more efficient healthcare system.
Improving Outcomes with AI-Assisted Interventions
The incorporation of AI into pediatric oncology is paving the way for improved patient outcomes, particularly in the realm of glioma treatment and recurrence prevention. By accurately identifying at-risk patients through advanced imaging techniques, providers can initiate timely interventions—whether they be adjustments to treatment plans or foundational lifestyle changes. This proactive strategy significantly contributes to minimizing the likelihood of relapse, ultimately enhancing the effectiveness of treatment protocols.
Moreover, AI-assisted interventions have the potential to optimize resource allocation within healthcare systems. By allowing more precise targeting of frequent monitoring for high-risk pediatric patients, resources can be conserved for those who truly need it, while simultaneously relieving the emotional burden on families of low-risk patients. In this way, AI not only improves clinical predictions but also transforms the overall healthcare experience for children battling cancer.
The Future of Pediatric Oncology with AI
The future of pediatric oncology looks promising with the integration of AI technologies. As more institutions embrace machine learning healthcare solutions, the potential for early detection and intervention in cancer recurrence will continue to grow. With ongoing advancements in algorithms and imaging techniques, researchers and healthcare providers are finding innovative ways to enhance patient care and develop personalized treatment plans for young oncological patients.
Moreover, as AI tools become standard practice, continued investment in research and development will be crucial. Bridging the existing gaps in knowledge and ensuring adequate training for practitioners in AI applications can further enhance the capabilities offered to pediatric cancer patients. Ultimately, the objective remains clear: to utilize AI in transforming not only the speed and accuracy of pediatric cancer diagnosis and recurrence prediction but also the entire healthcare experience for children and their families.
Machine Learning Advances in Pediatric Brain Tumor Treatment
Machine learning is revolutionizing the way pediatric brain tumors are treated. By analyzing large datasets from previous patient outcomes, these advanced algorithms can uncover correlations and patterns that might be overlooked by human analysis alone. The ability to glean insights from patient histories enhances the understanding of glioma treatment responses, guiding clinicians in choosing the most effective therapies tailored to individual patient profiles.
Additionally, machine learning models can help identify which patients may benefit from experimental treatments. Pediatric oncology is characterized by the need for innovative therapy routes, and AI can uncover new avenues for investigation, ultimately leading to a more refined approach to glioma management. As these technologies continue to develop, we can expect a future where treatments are driven by predictive analytics, heightening the efficacy of intervention strategies in the pediatric patient demographic.
Long-Term Monitoring and Supporting Families
Long-term monitoring for pediatric cancer survivors is crucial, yet often overwhelming for families. The psychological impact of constant monitoring and fear of recurrence can be taxing, creating a need for supportive structures within the healthcare system. By implementing AI-driven approaches focused on predicting relapse risks, healthcare providers can relieve some of the burdens families endure, providing more predictive clarity on when and how often monitoring is necessary.
Support systems will need to evolve alongside these advancements. Programs designed to educate families about the AI tools being utilized and how to interpret their significance can empower patients and their families. This empowerment leads to greater peace of mind, knowing they have a partnership aimed at navigating the complexities of pediatric cancer management, ultimately fostering a healthier, more optimistic outlook for the future.
Collaboration and Innovation in Pediatric Cancer Research
Collaboration across multiple institutions has been pivotal in advancing pediatric cancer research, particularly in the application of AI technologies. The convergence of expertise from various fields—radiology, oncology, and artificial intelligence—has resulted in a multi-disciplinary approach that enriches the research landscape. Such collaborations not only enhance the dataset available for AI training but also bring diverse perspectives that drive innovative ideas and solutions.
Innovations born from these collaborations, such as temporal learning models tailored for pediatric glioma predictions, exemplify the potential of collective effort in changing the landscape of pediatric oncology. By pooling resources and knowledge, these institutions are set to push the boundaries of what is possible in predicting and treating cancer in children, thereby ensuring a brighter, healthier future for young patients battling this disease.
Frequently Asked Questions
How does AI predict pediatric cancer recurrence more effectively than traditional methods?
AI predicts pediatric cancer recurrence by analyzing multiple brain scans over time, utilizing a method called temporal learning. This process allows the AI to identify subtle changes in imaging that indicate a risk of relapse, resulting in significantly higher accuracy compared to traditional single-scan methods.
What role does temporal learning play in predicting glioma recurrence risk in children?
Temporal learning enhances AI’s ability to predict glioma recurrence risk in pediatric patients by training the model to examine a sequence of MR scans taken over time. This approach captures the evolution of brain tumors, leading to more accurate predictions of whether cancer may recur after treatment.
What are the benefits of using AI in pediatric cancer treatment?
The benefits of using AI in pediatric cancer treatment include improved accuracy in predicting recurrence, reduced burden of frequent MR imaging for families, and potentially tailored treatment plans for at-risk patients. This advancements aim to enhance overall care for children undergoing treatments for conditions like brain tumors.
Can AI tools improve the management of pediatric glioma recurrence risk?
Yes, AI tools can significantly improve the management of pediatric glioma recurrence risk by providing earlier and more accurate predictions of relapse. This can lead to timely interventions and better-informed clinical decisions, potentially enhancing patient outcomes and quality of life.
What is the significance of the recent Harvard study on AI predicting pediatric cancer recurrence?
The Harvard study is significant as it demonstrates that AI can outperform traditional methods in predicting pediatric cancer recurrence, specifically in patients with gliomas. By utilizing nearly 4,000 MR scans, researchers showed that AI’s ability to learn from multiple images over time can markedly improve recurrence risk assessments.
How accurate can AI predict brain tumor treatment outcomes?
AI can predict brain tumor treatment outcomes with an accuracy ranging from 75-89% for gliomas, based on temporal analysis of post-treatment MR scans. This is a significant improvement compared to traditional methods, which had an accuracy of about 50%, illustrating the potential of AI in medical imaging.
What are the implications of using machine learning in healthcare for pediatric cancers?
The implications of using machine learning in healthcare for pediatric cancers include the ability to develop predictive models that enhance early diagnosis, personalized treatment strategies, and optimization of follow-up care. This can lead to more effective management of diseases like pediatric brain tumors, ultimately improving patient survival rates and quality of life.
What challenges exist in implementing AI for predicting pediatric cancer recurrence?
Challenges in implementing AI for predicting pediatric cancer recurrence include ensuring accuracy across diverse patient populations, validating the AI models in clinical settings, and addressing ethical concerns related to patient data usage. Ongoing research and clinical trials will be crucial to overcoming these hurdles.
| Key Points | Details |
|---|---|
| AI Tool Effectiveness | AI outperforms traditional methods in predicting pediatric cancer relapse risk, especially for gliomas. |
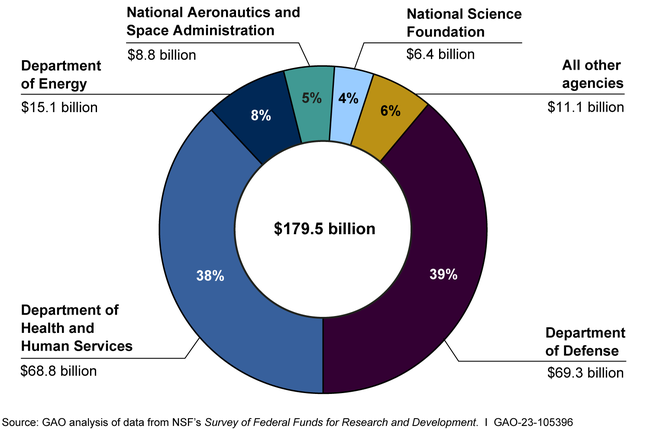
| Research Background | Conducted by researchers at Mass General Brigham, Boston Children’s Hospital, and Dana-Farber, involving 4,000 MR scans from 715 pediatric patients. |
| Temporal Learning | A novel approach that analyzes multiple brain scans over time to enhance prediction accuracy of recurrence. |
| Prediction Accuracy | The AI model predicts recurrence with 75-89% accuracy, significantly higher than the 50% accuracy of traditional methods. |
| Clinical Implications | Potential to reduce unnecessary imaging for low-risk patients and target treatment for high-risk individuals. |
Summary
AI predicting pediatric cancer recurrence represents a groundbreaking advancement in pediatric oncology. This innovative technology leverages temporal learning to analyze multiple brain scans, resulting in significantly improved prediction accuracy of cancer relapse. The findings from this research hold the promise of transforming patient care, potentially alleviating the burdens of frequent imaging while enabling timely and targeted interventions for high-risk pediatric patients.