Brain cancer prediction is evolving with the introduction of advanced artificial intelligence (AI) tools that significantly enhance our understanding of recurrence risk in pediatric patients. Recent research from Mass General Brigham demonstrates that machine learning in oncology can outperform traditional prediction methods by analyzing multiple MRI scans over time. This innovative approach aims to improve care for children facing pediatric gliomas, a group of brain tumors that, while often treatable, present varying risks of comeback. By integrating insights from numerous images taken post-surgery, these AI models provide a more accurate assessment of potential relapses, offering families hopeful news in a challenging medical landscape. As such technologies continue to develop, the future of brain cancer prediction looks brighter, promising better outcomes for young patients and their caregivers.
The landscape of oncology is shifting with groundbreaking advancements in brain cancer forecasting specifically aimed at pediatric patients. Utilizing sophisticated AI technologies, researchers are now better equipped to assess the likelihood of tumor recurrence in children diagnosed with brain malignancies such as gliomas. Through advanced imaging techniques like magnetic resonance imaging (MRI), these predictive models synthesize data from several examinations, enhancing accuracy beyond conventional methods. This transformative approach to detecting subtle changes in brain conditions over time not only alleviates some stress from frequent scanning for families but also optimizes treatment plans. As we witness the rise of these intelligent systems, the ability to accurately predict outcomes marks a vital progression in the fight against childhood cancer.
Understanding Pediatric Glioma: Challenges and Treatment
Pediatric gliomas present unique challenges in the field of oncology due to their complex nature and varied prognosis. These tumors, which originate in the glial cells of the brain, can significantly impact the lives of young patients. Treatment often involves surgical interventions, and while many gliomas are indeed curable through surgery alone, the concern of tumor recurrence looms large. Consequently, parents and healthcare providers must remain vigilant for any signs of relapse. This expertise is increasingly informed by advanced methodologies such as machine learning, offering innovative solutions to better predict outcomes.
Managing pediatric glioma requires a collaborative approach among specialists from different medical fields. Oncologists, neurologists, and radiologists work together to create a tailored treatment plan that considers the tumor’s characteristics and the child’s overall health. Additionally, new technologies, particularly artificial intelligence (AI), are enhancing predictive capabilities regarding treatment responses and relapse risks. By leveraging AI in cancer prediction, healthcare teams can optimize surveillance strategies, ensuring that children receive the best care possible while minimizing the emotional and physical burden of repetitive imaging.
The Role of AI in Brain Cancer Prediction
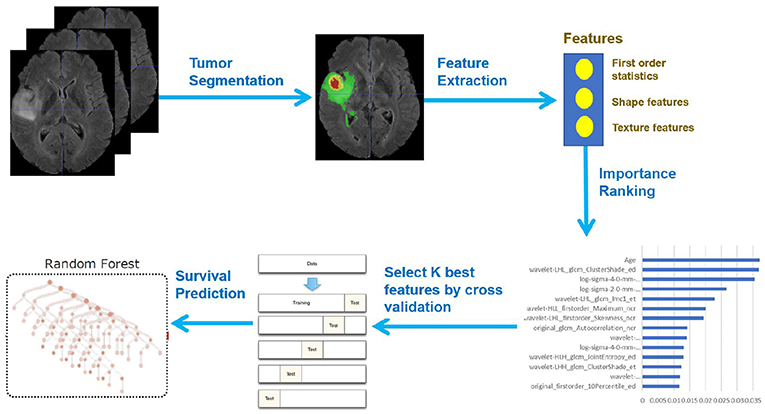
Artificial intelligence is revolutionizing medical diagnostics, and its application in predicting brain cancer outcomes is proving particularly beneficial. For pediatric patients battling gliomas, AI tools designed to analyze multiple MRI scans are outpacing traditional prediction methods, providing insights that were previously unattainable. The integration of machine learning techniques allows for greater accuracy in detecting subtle changes in scans over time, enhancing the potential for timely interventions when a risk of recurrence is indicated.
The Harvard study showcased how AI enhances the predictive power of recurrence risks in children diagnosed with brain tumors. By utilizing a method called temporal learning, AI systems can assess a series of MRI scans, capturing changes in the tumor’s environment that single snapshots may miss. This innovative approach represents a significant advancement in oncology, as it moves towards personalized medicine, enabling healthcare providers to adjust treatment protocols based on the individual patient’s risk profile.
Advancements in MRI Predictions for Brain Tumors
Magnetic Resonance Imaging (MRI) has long been a cornerstone in the diagnosis and monitoring of brain tumors. However, the advent of AI is transforming how these images are interpreted. Traditionally, radiologists reviewed each scan individually, which could lead to delays in identifying critical changes that signal tumor recurrence. With AI-enhanced tools, multiple scans can be analyzed simultaneously, allowing for a more comprehensive overview of a patient’s condition, which is vital for timely decision-making.
The use of advanced algorithms in MRI predictions offers a pathway to improved outcomes for children facing brain cancer. AI models trained on extensive datasets, like the nearly 4,000 scans from the recent study, learn to recognize patterns indicative of tumor behavior over time. This ability to predict potential relapses not only aids in immediate clinical decisions but also supports the mental well-being of both patients and families, alleviating the constant anxiety surrounding the unpredictability of cancer progression.
Optimizing Recurrence Risk Management in Children
Managing recurrence risk in pediatric glioma patients is essential for effective treatment and for maintaining a child’s quality of life. The fatigue and anxiety associated with multiple follow-up appointments and imaging tests can overwhelm families. Therefore, the integration of cutting-edge AI tools into routine care is a promising solution to improving monitoring processes. By identifying which patients are at the highest risk of relapse, healthcare providers can personalize follow-up schedules and minimize unnecessary burdens on young patients.
Furthermore, data revealed by AI models might empower healthcare teams to proactively implement strategies for those identified at high risk. Instead of relying solely on traditional imaging protocols, clinicians could initiate targeted therapies derived from AI predictions, significantly optimizing treatment pathways. As this research progresses towards clinical trials, the hope is for a system where anxiety surrounding potential recurrence is significantly reduced, enhancing the overall patient experience and health outcomes.
Future Directions for AI in Oncology
The potential of AI in oncology continues to expand, particularly in the realm of pediatric care. Researchers aim to refine AI models to include various forms of brain tumor data, not just gliomas. Future advancements could lead to comprehensive solutions that address all aspects of brain tumor management, from diagnosis to treatment and long-term follow-up. This holistic approach ensures that children receive personalized care based on their unique tumor characteristics and risk factors, leveraging machine learning to create a brighter future for pediatric oncology.
As these AI technologies mature, continuous collaboration among researchers, clinicians, and biotechnology companies will be crucial. Implementing robust clinical trials will validate AI predictions and establish guidelines for optimal practices in using AI for brain cancer prediction. With this cooperative effort, the vision of leveraging AI in clinical decision-making will soon transition from theory to routine practice, fundamentally transforming how pediatric brain cancers are diagnosed and treated.
Challenges in Implementing AI Technology in Healthcare
While the integration of AI in oncology promises numerous benefits, several challenges remain. Firstly, there is a need for high-quality data to train AI algorithms effectively; achieving this requires collaboration among hospitals and research institutions nationwide. Furthermore, concerns over data privacy and consent are paramount, particularly when dealing with sensitive medical records of minors. Addressing these challenges will be pivotal in establishing trust in AI systems among healthcare providers and patients alike.
Another challenge lies in the clinical acceptance of AI technologies. Many healthcare professionals may be hesitant to rely on AI-driven predictions without substantial validation from multiple clinical environments. Educating practitioners on the benefits and limitations of AI can lead to greater incorporation into everyday practice, ultimately aiding in better patient outcomes. As the dialogue surrounding AI in medicine evolves, it is essential to promote an understanding that AI acts as an adjunct to, rather than a replacement for, clinical judgment.
The Importance of Longitudinal Studies in Cancer Prediction
Longitudinal studies are essential in understanding the predictive patterns associated with pediatric glioma recurrences. By studying a cohort of patients over time, researchers can gather valuable insights regarding how tumors behave, how effective different treatment strategies are, and what factors contribute to relapses. This comprehensive understanding is particularly important in children, who may experience a different set of outcomes compared to adult patients due to their developing bodies and unique responses to treatment.
Additionally, integrating AI into longitudinal studies can enhance the precision of findings. As AI models learn from the evolving data collected over time, they can refine their predictions, leading to improved understandings of risk factors and tumor behaviors. Such insights will not only inform future research but also empower clinicians to tailor follow-up strategies effectively, ensuring that children with brain cancers have the best chances for long-term recovery without unnecessary emotional or physical strain.
Preparing for Clinical Trials in AI-Driven Oncology
The transition from research to clinical practice for AI-driven tools marks an exciting phase in oncology, particularly in managing pediatric gliomas. Preparing for clinical trials requires meticulous planning and collaboration among oncologists, radiologists, and AI specialists to ensure that trial protocols are robust. This includes establishing clear objectives for the clinical utility of AI predictions regarding recurrence risk, which are vital for the integrity and success of the trials.
Moreover, establishing parameters for patient enrollment will be crucial to interpret AI models accurately. Criteria may include tumor characteristics, treatment history, and demographic factors to provide a comprehensive view of each patient’s situation. Successfully navigating these preparatory steps will not only validate the use of AI tools in predicting brain cancer but may also pave the way for broader applications across various tumor types, reshaping the landscape of oncology.
The Future of Pediatric Cancer Care with AI
The future of pediatric cancer care is poised for transformation with the integration of AI technologies. As these tools evolve, we can expect more personalized treatment strategies that consider the individual characteristics of gliomas and other tumors. Enhanced predictive capabilities will enable clinicians to anticipate potential complications early and adapt treatment regimens accordingly. By leveraging artificial intelligence in cancer prediction, we can significantly improve the quality of life for young patients and their families.
Ultimately, the success of these advancements hinges on a collaborative effort among clinicians, researchers, and industry partners. Continued investment in AI technologies and their clinical validation will be essential to overcoming current challenges and realizing their full potential in enhancing patient outcomes. The intersection of artificial intelligence and pediatric oncology holds the promise of ushering in a new era of hope for children fighting brain cancer.
Frequently Asked Questions
How does AI improve brain cancer prediction in pediatric glioma patients?
AI enhances brain cancer prediction in pediatric glioma patients by analyzing multiple brain scans over time, achieving superior accuracy in predicting relapse risk than traditional methods. This approach, known as temporal learning, allows the AI model to recognize subtle changes in images taken post-surgery, improving the forecasting of potential cancer recurrence.
What role does machine learning play in predicting the recurrence risk in children with brain tumors?
Machine learning plays a critical role in predicting the recurrence risk in children with brain tumors by utilizing algorithms that learn from patient data, including MRI scans. These models can identify patterns indicative of relapse, leading to more accurate predictions and tailored follow-up care, especially in pediatric patients with gliomas.
Can MRI predictions for brain tumors help reduce the frequency of follow-up imaging?
Yes, MRI predictions for brain tumors, particularly when enhanced by AI, may help reduce the frequency of follow-up imaging by accurately assessing the risk of recurrence. If the AI identifies a lower-risk profile, families might experience less stress by minimizing unnecessary scans, while high-risk cases can be monitored more closely.
What is temporal learning and how does it aid in brain cancer prediction?
Temporal learning is a methodology used in brain cancer prediction that trains AI models to analyze multiple MRI scans taken over time. By organizing scans chronologically, the model can detect subtle changes that may signify cancer recurrence. This innovative approach significantly improves prediction accuracy for pediatric gliomas compared to analyzing single images.
What are the accuracy rates of AI in predicting pediatric glioma recurrence compared to traditional methods?
AI has demonstrated a remarkable accuracy rate of 75-89% in predicting the recurrence of pediatric gliomas, significantly outperforming traditional methods that only achieve about 50% accuracy. This advancement in brain cancer prediction represents a substantial improvement in patient management and care.
| Key Point | Details |
|---|---|
| AI Tool Effectiveness | AI predicts relapse risk in pediatric glioma patients more accurately than traditional methods. |
| Research Collaboration | Conducted by Mass General Brigham in collaboration with Boston Children’s Hospital and Dana-Farber/Boston Children’s. |
| Study Sample Size | Involved nearly 4,000 MR scans from 715 pediatric patients. |
| Temporal Learning Technique | Analyzes multiple brain scans over time, improving prediction accuracy. |
| Prediction Accuracy | Achieved 75-89% accuracy in predicting recurrence within one year post-treatment. |
| Need for Further Validation | Additional studies needed before clinical application to ensure safety and efficacy. |
| Future Clinical Trials | Planning trials to validate AI predictions for improving patient care. |
Summary
Brain cancer prediction innovations through AI tools mark a significant advancement in the healthcare field. Using multiple brain scans over time, researchers have enhanced the prediction of relapse risk in pediatric glioma patients, demonstrating that AI can outperform traditional methods. The study highlights the potential for AI to improve patient care by accurately predicting outcomes and personalizing treatment strategies, ultimately making the process less burdensome for families.