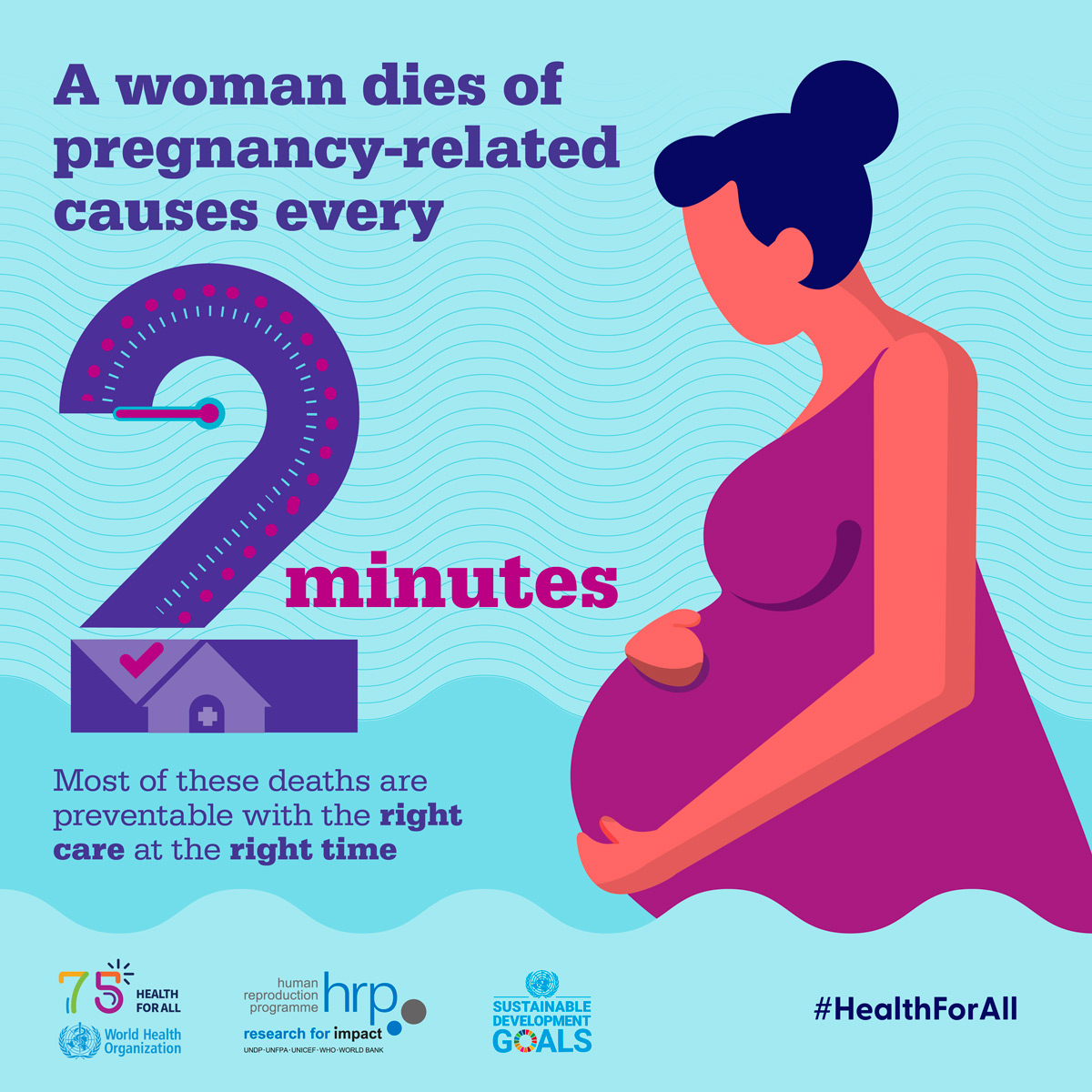
Maternal mortality remains a pressing issue in healthcare, particularly in the United States, where the rates of pregnancy-related deaths continue to rise alarmingly. Despite the fact that over 80% of these deaths are preventable, the U.S. still leads high-income countries in maternal mortality—a distressing statistic that highlights significant gaps in maternal health services. Studies show that from 2018 to 2022, the disparities in deaths among different racial and ethnic groups have only widened, with American Indian and Alaska Native women facing the steepest rates. Enhanced postpartum care and equitable healthcare policies are crucial in combating these preventable deaths and addressing the racial disparities in healthcare that exacerbate the crisis. As the nation grapples with these issues, it is clear that a comprehensive approach focusing on maternal health and informed policy changes is urgently needed.
The issue of maternal mortality is not just about numbers; it reflects the broader challenges surrounding pregnancy-related fatalities in the U.S. Often referred to as maternal deaths, these tragedies highlight systemic failures in our healthcare infrastructure, particularly regarding the care and support provided during and after pregnancy. Many women face maternal health disparities that contribute to a shocking increase in preventable deaths, influenced by factors such as access to necessary medical resources, quality of care, and societal inequities. This raises critical questions about postpartum care and the long-term health implications for mothers during recovery. Addressing these significant health crises demands immediate attention from policymakers and healthcare providers alike, ensuring that every mother receives the care she deserves.
Understanding the Rise in Maternal Mortality Rates in the U.S.
The United States has been facing an alarming rise in maternal mortality rates, which have hit a high compared to other high-income nations. Recent statistics show a significant increase in pregnancy-related deaths, with American Indian and Alaska Native women experiencing the highest rates. This trend is particularly concerning as it highlights underlying issues in maternal health and the systemic inequities present within the healthcare system. The rise is attributed to various factors, including the impact of chronic medical conditions, which are more prevalent among the population than in previous generations, thus posing a greater risk during pregnancy.
Additionally, the COVID-19 pandemic has exacerbated these trends, particularly in 2021, when the mortality rate peaked. The stark discrepancies in maternal mortality by race and state emphasize the need for comprehensive healthcare reform. Addressing these disparities is crucial not only for the health of mothers but for the well-being of their families and communities as a whole. The U.S. must learn from states that exhibit lower mortality rates, implementing policies and practices that prioritize maternal well-being and equitable care.
With the alarming statistics indicating that more than 80 percent of pregnancy-related deaths could be prevented, there’s an urgent call to action for improved prenatal and postpartum care. Many experts argue that addressing the gaps in maternal healthcare requires an intersectional approach that considers socioeconomic status, access to healthcare, cultural competence of healthcare providers, and community support systems tailored specifically to the needs of marginalized groups.
As attention turns to solutions, it’s clear that enhanced education for healthcare providers, investment in maternal health initiatives, and stronger advocacy for policy changes are necessary steps. Innovations in telehealth and extended postpartum support can significantly decrease mortality rates, offering mothers the proactive care they need during and after pregnancy.
The Role of Racial Disparities in Maternal Health
Racial disparities in maternal health are stark and alarmingly persistent in the United States. Research indicates that non-Hispanic Black women and American Indian women face morbidity and mortality rates far exceeding those of their white counterparts. These disparities are deeply rooted in historical and systemic biases within the healthcare system, leading to inequitable access to prenatal care, which significantly affects health outcomes. The correlation between race and maternal mortality is no coincidence; it reflects the broader socioeconomic factors that influence healthcare access and quality.
Efforts to address these disparities must focus on understanding the unique challenges faced by different racial and ethnic communities. Tailored healthcare initiatives that include cultural competency training for providers, community health education, and outreach programs can help bridge the gap. By fostering partnerships with local organizations that understand the specific needs of these communities, healthcare systems can begin to create a more equitable environment for mothers of all backgrounds.
Furthermore, policymakers must acknowledge and actively address the social determinants of health that disproportionately affect women of color. This includes ensuring that all populations have access to high-quality maternity care regardless of their socio-economic status or geographical location. Reducing racial disparities in maternal health not only saves lives but also contributes to healthier families and communities by promoting equity in healthcare.
The commitment to improving maternal health outcomes for marginalized groups will require sustained advocacy, funding, and innovative programming aimed at dismantling barriers to care. Only by addressing the intersectionality of race, health, and privilege can we hope to achieve a significant reduction in maternal mortality rates across diverse populations.
Preventable Deaths: A Call to Action for Maternal Health
Over 80 percent of pregnancy-related deaths in the U.S. are preventable, highlighting a crucial opportunity for intervention within maternal health systems. This statistic emphasizes the pressing need for improved education and access to healthcare resources for expectant mothers. Increasing awareness about warning signs during pregnancy and postpartum can empower women to seek help before complications arise, thus significantly reducing the number of preventable deaths associated with childbirth.
To address preventable maternal deaths, healthcare providers must implement standardized guidelines for prenatal and postpartum care, ensuring that women receive the comprehensive evaluations and monitoring necessary across their pregnancy journey. Additionally, increasing access to mental health resources and support during the postpartum period can help mitigate long-term complications and safeguard maternal well-being.
Through collaborative efforts among healthcare providers, policymakers, and community organizations, the nation can work towards sustainable improvements in prenatal care and postpartum support. Innovative solutions such as integrating technology for monitoring health and education, as well as investing in public health initiatives, can transform how care is delivered and accessed, ultimately decreasing preventable maternal deaths.
Ultimately, the focus must remain on a proactive approach to maternal health, identifying and addressing concerns early. By fostering an environment of awareness and support, we can evolve maternal healthcare in the U.S. toward a model that values and prioritizes the health of mothers and their children, paving the way for a healthier future across generations.
Postpartum Care: A Critical Component of Maternal Health
While prenatal care is vital for the health of mothers and babies, the importance of comprehensive postpartum care cannot be overlooked. The postpartum period, traditionally seen as a time for recovery, is often marked by physical and emotional challenges that can significantly impact a woman’s health. Over the years, data has highlighted that late maternal deaths—those occurring between 42 days and one year after childbirth—should be factored into discussions about maternal mortality. These findings underscore a crucial need for ongoing healthcare support that extends well beyond the delivery period.
Quality postpartum care can address various health issues, from managing chronic conditions like hypertension to providing mental health support. It’s essential to recognize that the postpartum phase is a continuum of care that deserves equal attention and resources as prenatal services. Comprehensive systems should be designed to ensure that mothers receive appropriate screenings, follow-ups, and interventions during this critical time to reduce morbidity and mortality.
Healthcare systems must adapt to this understanding by integrating postpartum care into their overall maternal health strategy, ensuring that mothers are supported physically and emotionally. Analysis of successful models that prioritize extended postpartum healthcare can inform best practices and encourage other regions to adopt similar initiatives. By fostering a holistic approach to maternal health, the healthcare system can significantly improve outcomes during the postpartum period.
Addressing the existing gaps in postpartum care not only supports mothers in their recovery but also has lasting benefits for families and communities as a whole. A commitment to enhancing postpartum care structures can transform maternal health outcomes, ultimately cultivating a safer and healthier environment for new mothers.
Addressing Healthcare System Inequities for Maternal Health
The issue of maternal mortality in the United States is inextricably linked to the nation’s fragmented healthcare system, which has led to significant inequities in access and quality of care. The lack of a cohesive approach to healthcare accessibility, especially in maternity care, has resulted in disparities across racial and geographical lines. These inequities create barriers that affect women’s health outcomes drastically, underscoring the need for systemic reform.
To build a more equitable healthcare framework, a multi-faceted approach is essential. Policymakers must prioritize investments in maternal health programs that target underserved communities, provide comprehensive coverage, and promote access to quality care. Ensuring that all women, regardless of their socioeconomic status or race, receive adequate medical attention during and after pregnancy is crucial for reducing pregnancy-related mortality.
Integrating community-based health initiatives that support equitable access to maternal care can significantly alter the landscape of maternal health. This includes increasing the number of healthcare providers in maternity care deserts and fostering partnerships with local organizations that advocate for maternal health. Furthermore, enhancing training for all healthcare professionals on implicit bias and systemic barriers can help create a more knowledgeable and sensitive workforce.
To effectively address healthcare inequities, collaboration between public health entities, state and federal policymakers, and healthcare providers is necessary. Continuous evaluation of healthcare systems and their impact on maternal health will steer initiatives in the right direction, ultimately fostering a more equitable landscape for all women.
Innovative Solutions to Improve Maternal Health Outcomes
Innovative solutions are crucial for tackling the escalating rates of maternal mortality in the U.S. As the healthcare landscape evolves, embracing technology and novel care models can redefine how maternity care is delivered. Telehealth services, for example, offer pregnant women remote access to healthcare providers, which can be particularly beneficial in rural areas where healthcare resources may be limited. This increased access supports timely interventions and fosters stronger healthcare relationships between patients and providers.
Additionally, implementing community engagement initiatives that involve expectant mothers in their healthcare decisions and education can empower them. Programs that educate women about the entire scope of maternal health—from pregnancy to postpartum care—create spaces for informed discussions about their health and encourage active participation in their care plans.
Moreover, focusing on preventive care through regular screenings and early interventions can significantly alter maternal health outcomes. Addressing chronic conditions like hypertension early on can prevent complications during pregnancy and reduce the risks associated with childbirth. Educational campaigns aimed at increasing awareness about maternal health issues can also play a pivotal role in promoting preventive measures and improving access to care.
Investing in research to identify the most effective interventions and best practices will provide the groundwork for developing efficient and targeted maternal health initiatives. By coupling innovation with evidence-based strategies, the healthcare system can transition toward a more proactive model that prioritizes the health and safety of mothers, ultimately lowering maternal mortality rates in the U.S.
Public Health Infrastructure: Building a Foundation for Maternal Health
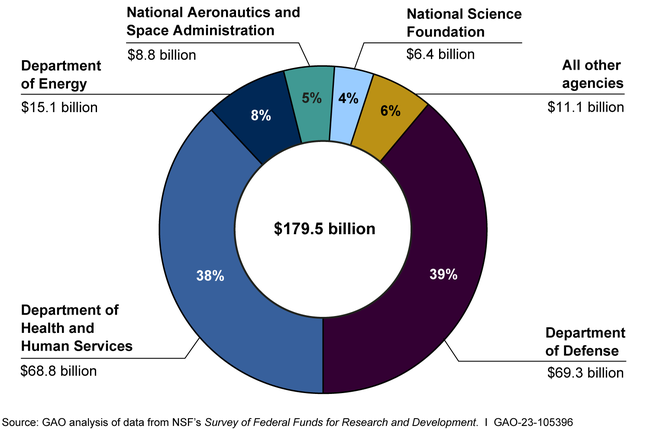
The strength of public health infrastructure is paramount in creating effective systems that support maternal health. A well-resourced public health system can facilitate the tracking of maternal mortality rates, ensuring that critical data informs policy decisions. Continuous investment in public health initiatives can better prepare states to address the healthcare needs of pregnant women and new mothers, ultimately lowering preventable maternal deaths.
Moreover, enhancing the capacity of public health agencies to understand and address the social determinants of health is essential for effective intervention strategies. This involves not only providing direct healthcare services but also creating supportive environments that foster health and wellness. Community engagement and partnerships with local organizations can enhance the reach and effectiveness of public health programs, ensuring that maternal health is prioritized across all communities.
Public health advocacy plays a crucial role in mobilizing resources and initiating reforms within the healthcare system. Amplifying the voices of women and families affected by maternal health issues can drive home the urgency for change and inform policymakers about the specific needs of underserved populations. By prioritizing maternal health in public health agendas, communities can work towards reducing health disparities and creating systems that support women before, during, and after pregnancy.
Ultimately, strengthening the public health infrastructure to address maternal health is not just about reducing mortality rates; it’s about nurturing healthier communities and future generations. Focusing on maternal health as a public health imperative will lead to a more equitable and compassionate healthcare landscape, preserving the lives of mothers and their children.
Frequently Asked Questions
What are the main causes of maternal mortality in the U.S.?
Maternal mortality in the U.S. is primarily caused by cardiovascular disease, accounting for over 20% of pregnancy-related deaths. Other significant contributors include hemorrhage and complications from chronic medical conditions, such as hypertension and diabetes. Preventable deaths during pregnancy are alarmingly high, with over 80% of such fatalities deemed avoidable.
How do racial disparities affect maternal mortality rates?
Racial disparities significantly contribute to maternal mortality rates, with American Indian and Alaska Native women experiencing the highest rates, nearly four times higher than white women. Non-Hispanic Black women also face disproportionately high maternal mortality rates. These disparities highlight systemic biases and inequities in maternal healthcare access and quality.
Why is postpartum care important in reducing maternal mortality?
Postpartum care is crucial in addressing maternal mortality as nearly a third of pregnancy-related deaths occur between 42 days and one year after childbirth, often due to complications that develop later. Improving access to comprehensive postpartum care can significantly reduce preventable deaths by addressing health issues that arise after the initial postpartum period.
What role does healthcare infrastructure play in maternal mortality?
The healthcare infrastructure plays a vital role in maternal mortality rates. Inadequate systems for monitoring and addressing maternal health needs contribute to preventable deaths. The U.S. needs to invest in public health infrastructure to ensure better quality care throughout pregnancy and the postpartum period, bridging gaps that exist across different states.
How can states improve maternal health outcomes?
States can improve maternal health outcomes by adopting best practices from higher-performing states like California, investing in healthcare infrastructure, and addressing policy differences that lead to disparities. Additionally, strategies must focus on innovative solutions that enhance quality of care during pregnancy and the postpartum phase.
What is the significance of tracking late maternal deaths in maternal mortality statistics?
Tracking late maternal deaths, which occur from 42 days up to one year postpartum, is significant because it recognizes that maternal health challenges extend beyond the early postpartum period. Understanding these deaths can lead to better healthcare system designs that encompass the continuum of care necessary for maternal recovery.
How does the COVID-19 pandemic influence maternal mortality rates?
The COVID-19 pandemic has influenced maternal mortality rates by exacerbating existing health disparities and hindering access to necessary care. Increased stress, delayed medical attention, and rising chronic health issues among pregnant individuals during the pandemic likely contributed to the rising rates of pregnancy-related deaths.
What measures can be taken to prevent pregnancy-related deaths?
To prevent pregnancy-related deaths, comprehensive measures must include enhancing prenatal care access, improving emergency interventions during pregnancy, and bolstering postpartum care. Additionally, addressing social determinants of health, such as racial inequities and access to healthcare, can significantly lower the rates of preventable deaths.
| Key Points | Details |
|---|---|
| U.S. Maternal Mortality Rates | The U.S. has the highest maternal mortality rate among high-income countries, which continued to rise from 2018 to 2022, peaking during the COVID-19 pandemic. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are deemed preventable, yet significant racial and regional disparities remain. |
| Disparities Across Demographics | American Indian and Alaska Native women have the highest mortality rates, nearly four times higher than white women. |
| Leading Cause of Death | Cardiovascular disease has become the leading cause of pregnancy-related deaths, surpassing hemorrhage. |
| Late Maternal Deaths | Late maternal deaths (deaths occurring between 42 days to 1 year postpartum) account for nearly a third of all pregnancy-related deaths. |
| Need for Improved Care | There is a critical need for better healthcare infrastructure and policies to address the rising maternal mortality rates. |
Summary
Maternal mortality remains a concerning public health issue in the United States, which has the highest rates among high-income countries. Despite the alarming statistic that 80% of pregnancy-related deaths are preventable, a recent study indicates these rates have continued to rise over recent years, with significant disparities noted across racial and geographic lines. Immediate action is needed to enhance prenatal and postpartum care, eliminate systemic inequities, and prioritize maternal health in policy discussions if we are to see tangible improvements in maternal mortality rates.